The Hidden Connection: Can Upper Cervical Misalignment Cause Tinnitus?
- New York UCC

- Feb 8
- 5 min read
Understanding the Link: Upper Cervical Misalignment and Tinnitus
For many, tinnitus is more than just a faint buzz; it is a relentless ringing, roaring, or hissing that interferes with daily life. While most people immediately consult an audiologist, the root cause isn't always in the ears. Emerging research and clinical success stories point toward a structural origin: upper cervical misalignment.
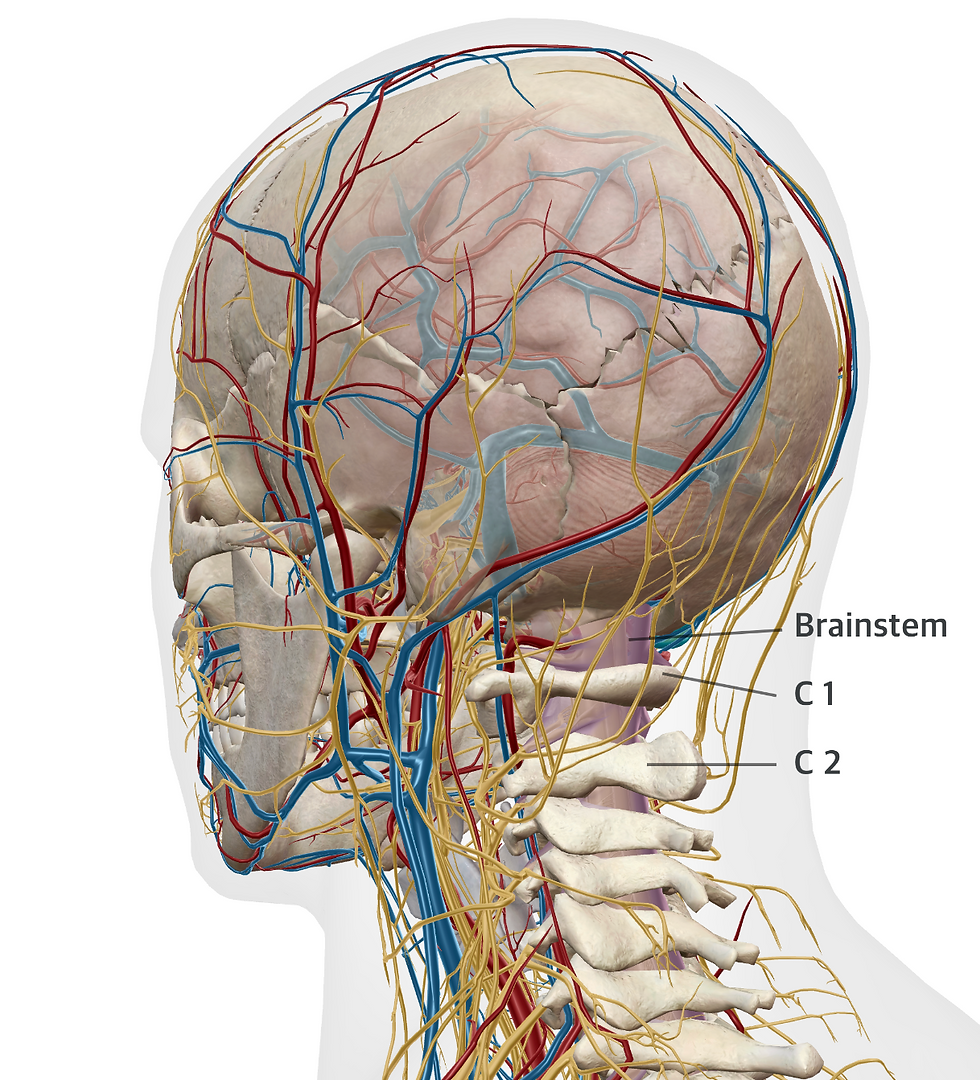
When the top two bones in your neck—the Atlas (C1) and Axis (C2)—shift out of their proper position, they can create a cascade of neurological and physiological stressors that manifest as phantom sounds in the auditory system.
The Anatomy of the Cranio-Cervical Junction (CCJ)
The cranio-cervical junction is the most complex and delicate area of the human spine. It houses the brainstem and sits in close proximity to several vital cranial nerves. Because the C1 and C2 vertebrae have the greatest range of motion, they are also the most susceptible to injury from whiplash, falls, or poor posture.

How the Upper Neck Can Influence Head and Ear-Related Symptoms
Many people are surprised to learn that the upper neck (upper cervical spine) plays an important role in how the brain processes signals from the head, face, and ears. While the neck does not control hearing directly, it can influence how sensory information is interpreted and regulated within the nervous system.
1. The Upper Neck and the Trigeminal System
The trigeminal nerve is the main sensory nerve for the face, jaw, temples, and much of the head. Sensory signals from this nerve are processed in the brainstem in an area that also receives input from the upper cervical spine (C1–C3).

Because signals from the neck and face converge in the same region of the brainstem, irritation or dysfunction in the upper neck can influence how trigeminal signals are perceived. This neurological overlap helps explain why problems in the neck may contribute to symptoms such as:
Headaches or head pressure
Facial pain or tightness
Pain around the eyes, jaw, or temples
Increased sensitivity in the head or face
This interaction is often described as trigeminocervical convergence, meaning that neck and head sensory pathways are closely linked at the brainstem level.
2. How Neck Function Can Influence Ear-Related Symptoms
Hearing and balance are primarily controlled by a separate nerve (the vestibulocochlear nerve). However, the brainstem acts as a central processing hub where information from the neck, jaw, balance system, and autonomic nervous system all interact.
When upper cervical input is abnormal, it can:
Alter brainstem sensory processing
Affect muscle tone and coordination in the head and neck
Influence blood flow regulation and nervous system balance
Because of this close integration, some people experience ear-related symptoms—such as pressure, fullness, ringing, or sound sensitivity—along with neck dysfunction, even though the neck itself is not responsible for hearing.


3. The Eustachian Tube and Muscle Coordination
The Eustachian tube helps regulate air pressure and fluid balance in the middle ear. It opens and closes with the help of small muscles that are involved in:
Swallowing
Jaw movement
Upper throat and neck coordination
When there is excessive tension or imbalance in the muscles of the jaw, upper neck, or throat, the Eustachian tube may not open and close as smoothly. This can contribute to sensations such as:
Ear pressure or fullness
Popping or clicking in the ears
Muffled hearing
Ringing or noise perception (tinnitus) in some individuals
These movements are coordinated by reflexes controlled through the nervous system. If nervous system regulation is disrupted, muscle coordination around the Eustachian tube may become less efficient.
Neurological and Physiological Mechanisms
The connection between the neck and the ears is largely "somatosensory." This means the brain receives sensory input from the muscles and joints of the neck that it then misinterprets as sound.
Neural Crosstalk: If the brainstem is under mechanical stress due to upper cervical misalignment, the dorsal cochlear nucleus (the "volume control" of the brain) can become hyperactive.
Blood Flow Restriction: The vertebral arteries pass through loops in the upper cervical vertebrae. A misalignment can subtly impede blood flow to the inner ear and the auditory cortex.
Cerebrospinal Fluid (CSF) Flow: Misalignment at the CCJ can act like a "kink in a garden hose," affecting the flow of CSF, which can increase intracranial pressure and cause pulsatile tinnitus.
How Common and Severe is it?
Tinnitus affects approximately 10% to 15% of the global population. For those with "Somatosensory Tinnitus"—tinnitus triggered by neck or jaw movement—the severity can be debilitating. Patients often report:
Inability to sleep or concentrate.
Co-occurring vertigo or dizziness (Meniere’s-like symptoms).
Severe migraines and "brain fog."
Neurological Conditions Linked to the CCJ
Beyond tinnitus, a chronic upper cervical misalignment can contribute to a variety of complex neurological conditions, including:
Trigeminal Neuralgia: Intense facial pain.
Post-Concussion Syndrome: Lingering headaches and cognitive issues.
Dysautonomia: Imbalances in the heart rate and blood pressure regulation.
Seeking Relief in New York
If you are struggling with persistent ringing in the ears, it’s time to look beyond the ear canal. At New York Upper Cervical Chiropractic, we focus on the precise correction of the cranio-cervical junction. Whether you are looking for an expert in Great Neck, or traveling from Long Island, Queens, or New York City, our goal is to restore your neurological health and silence the ring.
Frequently Asked Questions (FAQ)
1. How do I know if my tinnitus is caused by my neck? If your tinnitus changes in pitch or volume when you turn your head, clench your jaw, or apply pressure to your neck muscles, it is likely somatosensory and related to an upper cervical misalignment.
2. Can an X-ray show if my neck is causing ear ringing? Standard hospital X-rays often look for fractures or tumors. To see a subtle upper cervical misalignment, specialized 3D imaging (like Cone Beam CT) or specific Upper Cervical Chiropractic X-rays are usually required.
3. Is the adjustment for this area painful? No. Most upper cervical techniques are extremely gentle and do not involve the "cracking" or "popping" associated with general chiropractic.
4. How long does it take to see results? Neurological healing takes time. While some feel immediate relief, most patients notice a gradual reduction in the intensity and frequency of the ringing over several weeks of stabilization.
5. Can this help with Meniere’s Disease? Yes. Many cases of Meniere’s involve both tinnitus and vertigo, both of which have been clinically linked to dysfunction at the cranio-cervical junction.
📍 505 Northern Blvd, Ste 309, Great Neck, NY 11021
📲 516) 969-3330